- Reduces redundancy and manual effort,
- Fits into real clinical workflows, and
- Supports both patient and provider outcomes without inflating cost or complexity.
The healthcare industry in the U.S. and globally isn’t short on software, it’s short on software that works.
After years of hurried digital adoption, especially post-2020, healthcare organizations are stepping back and asking a harder question: Are our systems helping us deliver better care or just adding another layer of complexity?
Spending continues to rise. The U.S. healthcare IT market alone is projected to reach $325 billion by 2033, growing at a steady 13.1% CAGR, according to IMARC Group. But investment doesn’t guarantee impact, especially when the wrong tools are prioritized.
Meanwhile:
More than 50% of U.S. healthcare providers say their existing software tools don’t integrate well with others.
Administrative burden remains the #1 cause of physician burnout, with over 60% of clinicians citing inefficient EHR workflows as a contributing factor.
On the patient side, expectations have changed: 3 out of 4 patients now prefer digital communication and remote monitoring over in-person visits for routine care.
In 2025, the focus has to shift toward software that:
This blog doesn’t just list tools. It identifies 10 software types that are solving real problems today and where healthcare organizations should actually be looking when working with a healthcare software development company.
The challenges in healthcare today aren’t new but the urgency to solve them is sharper than ever. Burnout, inefficiencies, data silos, rising costs, and inconsistent patient experiences are no longer issues to “monitor.” They’re make-or-break factors for providers, payers, and innovators alike.
This is where smart, well-designed software comes in, not as a magic fix, but as a tool that, when done right, supports real care delivery and operational performance.
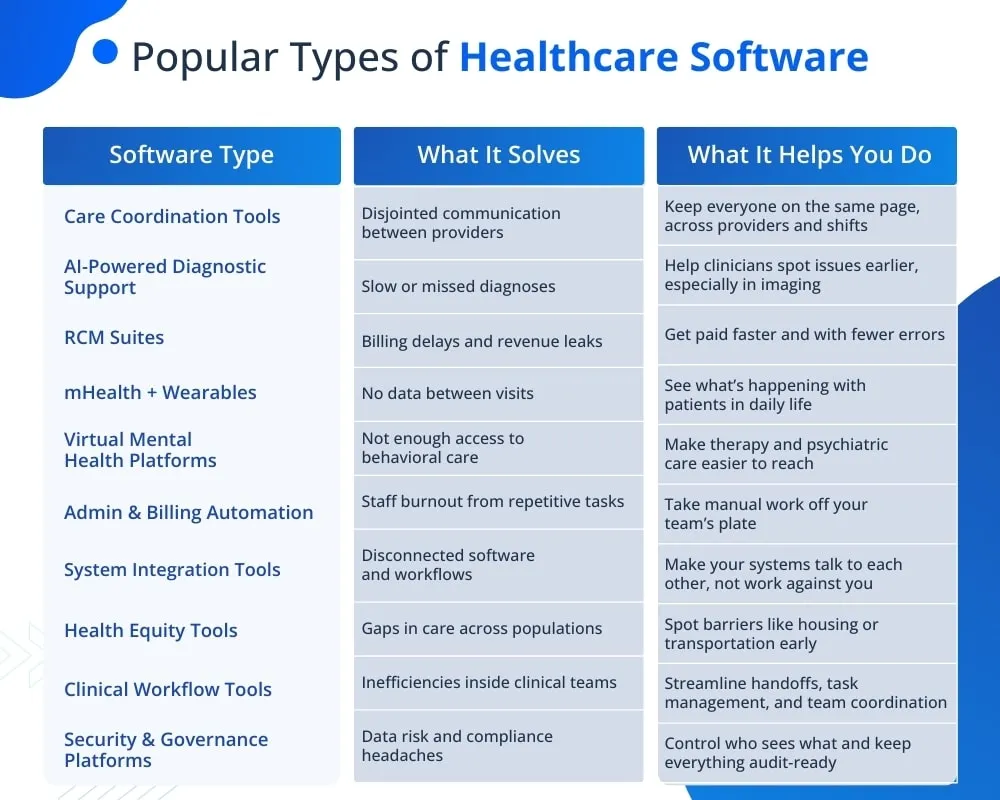
Below, we break down 10 types of healthcare software that are not just trending, they’re being used right now to solve actual problems for healthcare organizations across the U.S. and globally. Each one is grounded in real-world demand, not just hype.
Disjointed communication across providers leads to redundant tests, treatment delays, and increased readmissions. Care fragmentation costs the U.S. healthcare system over $78 billion annually (JAMA).
Care coordination platforms close the communication loop between physicians, specialists, nurses, and case managers, helping everyone stay on the same page, literally.
What These Tools Help With:
The global care coordination software market is projected to grow from $7.5B in 2023 to $17.2B by 2030, at a 24.5% CAGR.
✅ Interoperability with EHRs
✅ Intuitive, non-clinical UI
✅ Secure messaging & task tracking
✅ Built-in analytics & compliance support
Healthcare systems lose valuable time and accuracy in diagnosis due to overburdened radiologists, manual image interpretation, and growing clinical data complexity. Misdiagnosis or delayed detection remains a leading contributor to poor outcomes and unnecessary costs.
AI-powered diagnostic tools help clinicians interpret medical images and patient data faster and more accurately. They analyze scans, detect anomalies, and surface insights that improve triage and treatment planning, especially in radiology, oncology, and pathology.
What These Tools Help With:
The global AI in medical diagnostics market is projected to grow from $1.77B in 2025 to $14.46B by 2034, at a 27.1% CAGR.
✅ Compatibility with PACS and EHRs for seamless data integration
✅ FDA-cleared or CE-marked algorithms for clinical use
✅ Real-time alerting for critical findings
✅ Continuous model improvement as new data is fed
✅ Audit trails and explainability features for clinician confidence
The business side of healthcare is complex, and mistakes are expensive. Claims get denied, coding is inconsistent, and reimbursements take weeks or months to arrive. These delays and gaps directly affect operating margins, especially for organizations balancing high patient volumes with thin financial buffers.
RCM suites give healthcare providers better control over how revenue moves through the system. They help staff work faster, reduce errors, and recover income that might otherwise be lost. Whether you’re managing a private practice or a hospital network, having clean, accurate financial processes in place matters and so does being able to measure and improve them.
What These Tools Help With:
The global RCM market is expected to grow from $169.69B in 2025 to $451.29B by 2034, at an 11.5% CAGR.
✅ Integration with your clinical documentation and EHR
✅ Eligibility and coverage checks that run before services are rendered
✅ Charge capture tools tied directly to care workflows
✅ Claim scrubbers that flag issues early
✅ Transparent reporting for finance, not just billing
Most health data is still captured inside the clinic. That leaves a wide gap between visits, especially for patients managing chronic conditions or recovering at home. Without a clearer picture of what’s happening day to day, providers are forced to guess, and patients often disengage.
mHealth apps paired with wearables give providers access to what’s happening between appointments. Heart rate, sleep, activity, glucose, symptoms in real time or close to it. For patients, it means fewer surprises, better habits, and a stronger connection to their care team.
What These Tools Help With:
The global mHealth apps market is projected to grow from $63.5B in 2023 to $243.57B by 2030, at a 21.2% CAGR
✅ Integration with consumer and clinical wearables (e.g. Apple Watch, Dexcom, Withings)
✅ Secure data sharing that meets U.S. regulatory standards
✅ Interfaces designed for non-technical users
✅ Metrics that are actually actionable, not just charts
✅ Ability to flag trends or outliers without manual review
Access to therapy and psychiatric care is limited by geography, cost, and provider shortages mainly outside major cities.
Virtual platforms give people direct access to licensed professionals, without the barriers of location, waitlists, or stigma.
What These Tools Help With:
The global virtual mental health market is projected to grow from $5.8B in 2023 to $22.7B by 2030, at a 21.3% CAGR
✅ Secure video and messaging for one-on-one or group sessions
✅ Support for both synchronous and asynchronous care models
✅ Built-in screening tools (e.g. PHQ-9, GAD-7)
✅ Mobile-first design for private, stigma-free access
✅ Integrations with EHRs or primary care referrals
Clinicians and admin staff are spending too much time on repetitive tasks, from billing follow-ups to patient intake. It’s inefficient, error-prone, and one of the top contributors to burnout.
Automation tools handle the tasks that don’t require human judgment, freeing up time for work that actually does like care delivery, patient support, and complex problem-solving.
What These Tools Help With:
The healthcare automation market is expected to reach $91.6B by 2032, growing at a 10.3% CAGR, with billing and admin automation among its fastest-growing segments
✅ Rules-based workflows that manage approvals, edits, and escalations
✅ Digital forms and pre-visit check-ins that cut wait times
✅ Coding automation with built-in error detection
✅ Secure task routing for billing, scheduling, and documentation
✅ Dashboard-level oversight for operations and admin performance
Healthcare runs on fragmented systems like EHRs, labs, imaging, billing, many of which don’t communicate well. That disconnect slows down care, creates administrative friction, and risks patient safety.
Integration tools bridge the gap between systems that weren’t built to work together. They enable timely data exchange across departments, vendors, and even care settings without requiring everything to be rebuilt from scratch.
What These Tools Help With:
The healthcare interoperability solutions market is projected to grow from $3.4B in 2023 to $8.7B by 2030, at a 14.4% CAGR
✅ Standards-based APIs (HL7, FHIR) for vendor-neutral data exchange
✅ Data mapping and transformation between format
✅ Integration engines that sit between systems and not replace them
✅ Real-time sync options where batch processing won’t do
✅ Visibility into data flows, errors, and audit trails
Healthcare isn’t evenly distributed. Where patients live, what language they speak, or whether they can get to a clinic all influence outcomes and most systems aren’t equipped to track or respond to that.
Health equity tools give care teams visibility into social factors that affect patient health. That insight helps them deliver care more effectively and build programs that actually reach the people being left out.
What These Tools Help With:
The global SDOH analytics market is projected to grow from $4.4B in 2023 to $16.3B by 2030, at a 20.6% CAGR
✅ Built-in SDOH data fields aligned with U.S. core standards
✅ Integration with community resource directories and referral networks
✅ Patient segmentation tools by ZIP code, income, or access risk
✅ Visual dashboards to track disparities and program impact
✅ Support for compliance reporting (e.g., HRSA, NCQA, CMS equity measures)
Too much of a clinician’s day is spent on tasks that don’t require a medical degree such as chasing records, navigating multiple systems, or managing handoffs that should be automatic.
Workflow tools help healthcare teams spend less time coordinating and more time delivering care. They organize tasks, streamline documentation, and reduce the friction that slows everyone down.
What These Tools Help With:
The global clinical workflow solutions market is expected to reach $23.7B by 2030, up from $9.6B in 2022, growing at a 12.2% CAGR
✅ Role-based task lists and activity tracking
✅ Alerts for time-sensitive tasks or pending documentation
✅ Visual boards for team-based coordination
✅ EHR integration for seamless data flow
✅ Reporting tools to monitor process efficiency
Healthcare data is a top target for breaches and a single compliance failure can lead to millions in fines, lost trust, and operational fallout.
Security and governance tools give healthcare organizations control over how data is accessed, shared, stored, and audited. In a system built on trust, protecting information is protecting care itself.
What These Tools Help With:
The healthcare cybersecurity market is projected to grow from $18.2B in 2023 to $57.25B by 2030, at a 17.8% CAGR
✅ Centralized access control and identity management
✅ Automated compliance tracking and documentation
✅ Encryption and endpoint protection across devices
✅ Real-time alerts for breach attempts or policy violations
✅ Built-in audit logs and reporting for regulators and internal review
In 2025, healthcare leaders aren’t looking for more software, they’re looking for better decisions. The real questions are practical: What’s worth building? What can be integrated? What’s adding complexity instead of solving problems?
Strong teams don’t chase features, they prioritize outcomes. And the right software development partner doesn’t start with a product roadmap. They start with a clear understanding of how care is delivered, how systems operate, and where friction actually exists. From there, the focus is simple: build only what matters, and make sure it works in the real world.
There’s no universal software stack that fits every healthcare organization. What works in a large health system doesn’t always work in a specialty practice. What solves one team’s pain point might overload another. That’s why successful healthcare software in 2025 and beyond starts with a much simpler question: What problem are we trying to solve?
The ten software types in this blog aren’t trends for the sake of staying current. They’re answers to the actual pressure points care teams, operations, and leadership face every day: rising costs, inefficient handoffs, disconnected systems, staff fatigue, and limited access to care.
For healthcare software development to create real value, it has to stay rooted in the day-to-day. That means building tools that reduce friction instead of adding features for their own sake. It means designing for the people who use the system, not just the ones who approve the budget. And it means knowing when to build, when to integrate, and when to say no.
The software that makes the biggest difference in 2025 won’t necessarily be the most advanced. It will be the most aligned with your workflows, your patients, and your goals.

If you’re planning a new platform or fixing what’s already in place, choose a healthcare software development company in the USA in the USA that knows where to focus. We don’t just build software, we help you solve the right problem, with the least complexity.
Talk to our team and let’s build something that works: for your system, your staff, and your patients.
Are You Prepared for Digital Transformation?
Software Development
Discover the best low-code development platforms and real-world use cases helping USA businesses build custom software faster.
Fintech
Explore how fintech software is built in the USA, from core features and compliance to architecture, development costs, and the latest trends driving financial innovation.
Software Development
Ready to build smarter real estate tech? Discover how PropTech software can boost efficiency, streamline workflows, and meet U.S. market demands. Let’s get started!